News
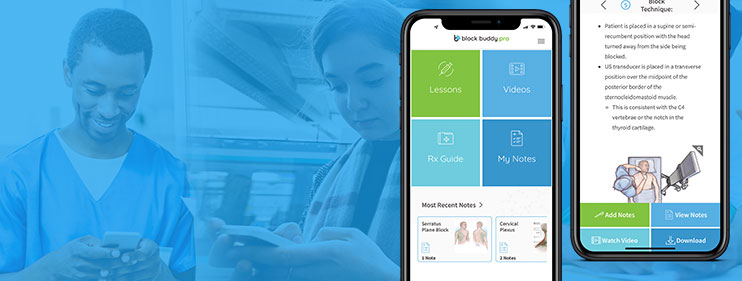
Major Update: Introducing the New and Improved Block Buddy Pro App
Major Update: Introducing the New and Improved Block Buddy Pro App We are thrilled to announce the release of a…
Read MoreHow To Sign Up For Block Buddy Pro
If you are a CRNA, SRNA, or other kind of anesthesia provider, you may be interested in the Block Buddy…
Read MoreRegional Nerve Blocks Are The Non-Opioid Alternative For Chronic Pain Relief
America’s Worst Drug Epidemic in History: The Opioid Crisis We are in the middle of one of the deadliest epidemics…
Read MoreBlock Buddy Pro Resident Discount
Residents Exclusive Offer: Affordable Pricing Just for You! No matter how you look at it, going to college is not…
Read MoreGlobal Response Management Partners With Block Buddy Pro
Block Buddy Pro is partnering with Global Response Management to provide education about ultrasound guided nerve blocks to high-risk, low-resource areas. The Block Buddy Pro mobile app will be utilized by GRM medics in the field when performing life-saving operations across the globe.
Read MoreHost Customized Regional Anesthesia Conferences
Continue Education with Custom Conferences Continuing education has never been more convenient! Block Buddy offers private workshops and conferences with award-winning, world-class…
Read MoreHow To Safely Dispose Of Opioids And Pain Medication
Do you have old opioids or pain medications in your medicine cabinet that you no longer use? As many as 92…
Read MoreGive The Gift Of Education
The Perfect Gift for a CRNA or Anesthesiologist We all have certain friends or family members who are difficult to buy…
Read MoreBlock Buddy Co-Owner Receives Anesthesia Award
Block Buddy co-owner Scott Urigel was honored with the 2019 Alice Magaw Outstanding Clinical Anesthesia Practitioner Award. “It was an honor and…
Read MoreIt’s Here!
The owners and creators of Block Buddy, Scott Urigel and Jeff Molter, are elated to announce the launch of the…
Read MoreNew Guidance Outlines Recommendations For Infection Control In Anesthesiology
Press Release: The Society for Healthcare Epidemiology of America, December 2018. Arlington, Va. — The Society for Healthcare Epidemiology of…
Read More